While the odds are that a low-FODMAP diet will help you feel better, irritable bowel syndrome (IBS) is a complex condition. It wouldn’t be realistic to expect a single solution to work for everyone. There will be some people who do not get significant relief of IBS symptoms during the elimination phase of the low-FODMAP diet. The fact is, sometimes it isn’t about the food. And if it is about food, sometimes it isn’t about the FODMAPs. Before moving on, though, consider these questions. Perhaps some fine-tuning, a FODMAP re-do, or a meeting with a registered dietitian would help you get better results.
Did you forget the IBS basics? Traditional advice for IBS wasn’t all bad. Even on a low-FODMAP diet, it’s important to drink enough water, avoid overeating, eat good sources of dietary fiber, and get some regular exercise. Sometimes I see my patients have cut out high-FODMAP beverages and forgotten to replace them with low-FODMAP teas or cold drinks. Or they’ve not replaced the high-fiber Brussel’s sprouts, cauliflower, and cashews they were eating with good low-FODMAP sources of fiber.
Did you follow advice from a qualified expert? Who prepared the tools you used for your low-FODMAP diet? Who helped you with strategies for success? If you aren’t in a position to get in-person help from a qualified health care professional such as a registered dietitian, you should at least be reading advice written by one. The best patient-advocate bloggers, recipe developers, and health writers know this, and partner with nutrition professionals to provide scientifically accurate, credible information.
Not every dietitian is knowledgeable about FODMAPs. Some are generalists or may specialize in treating other health conditions, such as diabetes or cancer. It wouldn’t be reasonable to expect them to know all the nuances of low-FODMAP diets. Be sure you have been advised by someone who specializes in special diets for gastroenterology patients.
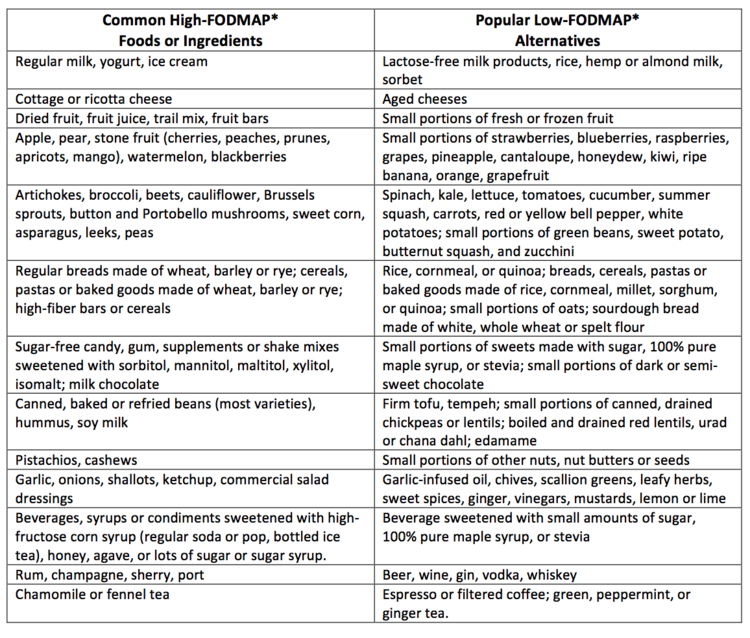
Did you use complete and up-to-date lists of high- and low-FODMAP foods? Even tools prepared by credible experts can be woefully out of date due to rapid changes in this still-new field. For example, one 2012 food list from a credible, big-name university is still circulating on the internet via third parties, though I suspect the authors of that handout have probably revised it several times since then. And some one-page handouts (like mine) were never meant to be complete lists, but to illustrate the highlights of high- versus low-FODMAP foods.
Did you eat moderate-FODMAP foods too often, or in large portion sizes? Most food lists and apps do have some way to indicate foods that are only low-FODMAP in small portions. In my book, The IBS Elimination Diet and Cookbook, these foods are in bold font and have a portion size indicated. All fruits are in this category, for example, blueberries, ½ cup.
It is more difficult to communicate how to avoid so-called “FODMAP stacking.” With many tools and apps, there is really nothing stopping you from eating too many of these portion-controlled foods at once. If you make a smoothie with ½ cup each of 4 different kinds of moderately-low FODMAP fruit, is the smoothie low in FODMAPs? No. If you have 2 cups of oatmeal topped with 1 cup of blueberries, 2 tablespoons of brown sugar, and some walnuts, is that still a low-FODMAP meal? No, even though you may find all of those foods are “allowed” on various lists of low-FODMAP foods. The program in my book recommends limiting yourself to two bold portions per meal or snack, to keep it low-FODMAP.
Were you already eating a low-FODMAP diet before you began? Some people with IBS have been avoiding high-FODMAP foods for years, before they ever heard the term. If you routinely avoided dairy products, gluten, beans, onions and other “gassy vegetables” and nuts because they bothered you, you may experience less dramatic improvement on a low-FODMAP diet—there wasn’t much room to move! You can still get two important benefits from this process. First, complete low-FODMAP food lists might help you eat a wider variety of foods that won’t trigger your IBS. Second, during the next step (the reintroduction process) you might have some pleasant surprises. You may find that you can tolerate some small to moderate amounts of certain FODMAPs when the other foods you are eating are low in FODMAPs. Something to look forward to!
If you followed a low-FODMAP diet closely, using excellent tools, you and your dietitian might want to consider whether other types of adverse food reactions might be affecting you. Several of the most common non-FODMAP issues are intolerance to high-fat meals, and dairy or gluten sensitivity.
You may also need to have another conversation with your doctor about non-food issues contributing to your diarrhea, constipation, abdominal pain, excess gas or bloating. A partial list to consider would include another gastrointestinal condition, medication side effects, stress, motility problems, or gynecological problems.
This page may contain affiliate links. We are a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for us to earn fees by linking to Amazon.com and affiliated sites.